The final 2026 Star Ratings were released on October 9, 2025. Among the health plans rated in both 2025 and 2026:
- 45% maintained their overall Star Rating
- 29% declined by at least half a star
- 26% improved by at least half a star
The average overall Star Rating continued its gradual decline, decreasing from 3.67 to 3.65.
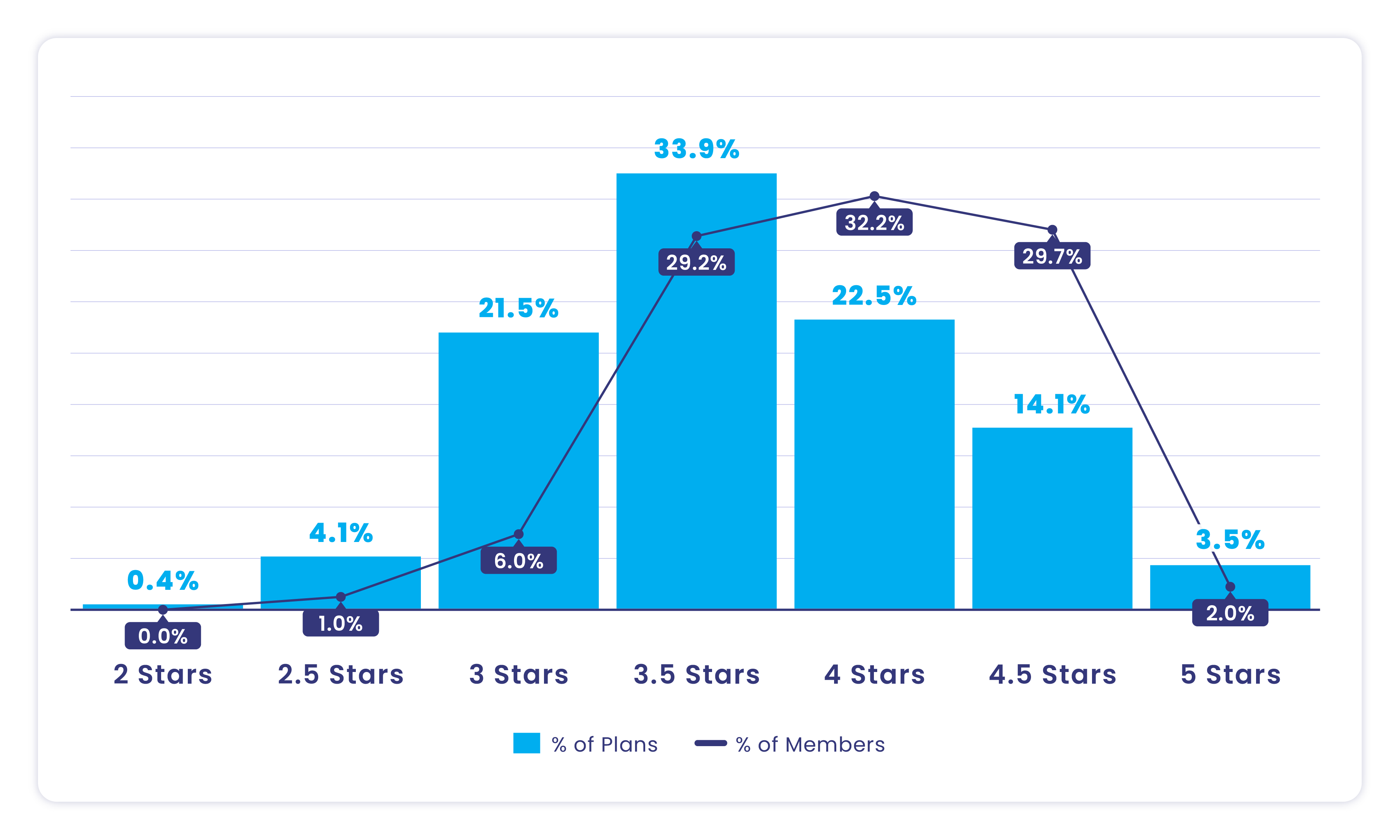
Approximately 40% of contracts offered in 2026 achieved 4 Stars or higher, spanning more than 75% of states, with an average plan size of 10,000 members. Over 60% of members are enrolled in 4+ Stars health plans. All five-star plans for SY26 are special needs plans (SNP) with an even distribution of plans that have been in the industry less than five years, 5-10 years, and over 10 years.
The key takeaways from the top performing health plans are:
- Quality improvement measures helped plans reach five stars
- The top three performing measures were Eye Exam for Patients with Diabetes, Diabetes Blood Sugar Control, and Care for Older Adults: Medication Review (SNP only measure).
Performance results indicate that both small and large health plans can achieve 5-Star ratings, suggesting that plan size is not a key driver of success. One additional key takeaway is that states with 5-star plans also have 3-star or lower plans, showing that success is not driven by geography — it’s driven by effort, strategy and sustained investment in quality improvement. Plans that consistently put in the work to strengthen measure performance see a clear return on resource and budget investment.



The upward movement of cut points in transitions of care measures, including Plan All-Cause Readmissions and Follow-Up After ED Visit for members with multiple high-risk chronic conditions, indicates that industry-wide performance is improving. To keep pace with these higher performance thresholds, health plans must continue to strengthen and invest in transition-of-care programs that support member coordination and continuity.
SY2027 impact
Several upcoming changes for Star Year 2027 will impact overall performance for health plans:
- The Reward Factor will be removed and replaced with the Excellent Health Outcomes for All (EHO4All) reward which will have a more positive impact for health plans with disabled, low-income status and dual eligible members. It may negatively impact health plans that received 4+ Stars due to the additional support from the reward factor.
- The Eye Exam for Patients with Diabetes HEDIS measure will change to an Electronic Clinical Data System (ECDS) measure. This measure was a top performing measure for five-star plans and it will be key to track performance without the hybrid approach.
- The Health Outcomes Survey (HOS) measures, Maintaining or Improving Physical Health or Mental Health, are increasing from one weigh to three weight measures.
What should health plans focus on
While we await further guidance from CMS in the Final Rule, payers should focus on three areas in MY2026:
- Reset your goals based on the updated cut points with room for further improvement based on prior year cut point trends.
- Update your dashboards to make sure they do not include the Reward Factor and focus on reaching your Star Ratings goals without it.
- Continue to assess and improve access to real time data from your provider systems to identify clinical gaps, not data gaps, as we continue to transition to ECDS measures.
{{cta}}
How can health plans improve with limited resources
All health plans are pulling back resources to prepare for additional changes in government spending. However, this cannot change the goal of supporting members to improve their health outcomes. The following next steps are best practice to keep up with the changes with limited resources:
Leverage community partnerships:
- Strengthening partnerships with provider health systems, community-based organizations, and other community support programs offers a practical and impactful way to connect with and support members throughout their health care journey. An example of this type of partnership is organizing who follows up with members after an inpatient discharge. Coordinate communications across the health plan, health system, and vendors to minimize member confusion and outreach fatigue.Another example is coordinating orders for screenings with providers to help streamline scheduling preventive screenings without barriers. Work with your providers to make bulk orders for lab work, outpatient testing (mammograms), and at home testing (Cologuard). Find out how Healthmine is helping plans increase completions of Cologuard kits.
- Partnering with Aging and Disability Resource Centers (ADRCs) can help members access in-home meal programs, ensuring that high-risk or homebound members receive nutritional support. This approach not only addresses social determinants of health but also reduces the need for multiple, fragmented touchpoints, creating a more coordinated and supportive member experience.
Increase communication options
Work with engagement vendors to understand how best to communicate with your population — and follow through. The additional options are not only a preference but can also be the best communication option for members with communication constraints that require specific technology, such as texting. We’re seeing a growing percentage of aging adults prefer digital options for engaging with their plan. They’re doing more than ever on smartphones. These options are no longer innovative and are now best practice as they become expected by your members.
As CMS transitions toward ECDS reporting, which emphasizes capturing data across the entire member population rather than a traditional hybrid sample of 411 members, broad-based engagement becomes critical. Effective population health strategies — such as SMS reminders, digital surveys, and proactive care gap notifications — help ensure that all members are reached and engaged in their care.
Health plans that leverage these modern, data-driven communication tools will be better positioned to close care gaps at scale, improve ECDS performance, and meet member expectations in an increasingly digital environment.
3 ways Healthmine is helping payers improve scores
Healthmine has a proven track record of improving Star Ratings scores. In SY26, 30% of Healthmine’s on-platform clients achieved 4 stars or higher.
- Expert-driven outreach: Not all outreach is created equal, and not all teams are equally as equipped to develop member outreach, especially when you’re chasing a very specific goal — like measure-level improvement. Our team is better positioned to help you understand your biggest areas of opportunity, develop a plan to achieve it and then implement the right member outreach to get you there. Our teams bring experience as health plan leaders of former 5-star plans, behavioral science backgrounds and visibility to the bigger picture of your priorities and the member experience, which payer marketing teams often lack or don’t have resources to pursue most effectively. Need proof? Here’s how we’re approaching quality and risk outreach more strategically (and with better outcomes).
- Smarter rewarding: Rewards help bridge the gap between a need and an action. But generic incentive programs typically waste dollars, effort and don’t yield the right results. Separately, most reward vendors take weeks to fulfill incentives, causing abrasion, increased call volume and decreased member satisfaction. Our programs are different — uniquely designed to your goals so you’re incentivizing the right actions only and targeting the members who you need to activate the most. Plus, our digital rewards are delivered within 48 hours of redemption, so your members are never left wondering, “Where’s my reward?” Read more about common pitfalls with reward programs and how we solve them.
- Closed-loop engagement: We’ve brought data and analytics, timely health actions, appointment scheduling and appointment follow-up into one, closed-loop experience for members. Health plans can notify members they’re due for provider visits, use AI-supported provider matching and appointment scheduling to get members into their doctor’s office without ever having to make a phone call, then send follow-up directing the member to their next best health action. Want to try it out? Take a tour of provider matching and scheduling with this interactive experience.
Don’t miss out on opportunities to improve performance in MY26. Find out how Healthmine can bridge the gap between engagement and meaningful Stars results. Contact us today.
Summary
- The 2026 Medicare Star Ratings show an increase in five-star plans and a consistent percentage of plans reaching 4+ stars from SY25 to SY26. Results have also demonstrated the importance of leveraging the quality improvement measures to reach Star ratings goals.
- Upcoming 2027 rules will reshape performance. Major updates include replacing the Reward Factor with the EHO4All reward, transitioning the Diabetes Eye Exam to an ECDS measure, and tripling the weighting of HOS measures. These will significantly impact plan scoring and strategy.
- To adapt with limited resources, health plans should focus on member-centered communication with a window into the best times and opportunities to engage members. This will drive quality improvement and maintain or improve Star Ratings.

.svg)
Webinar: From Stars to Strategy
How to use SY26 to build actionable, data-driven strategies for the next Stars measurement year.


.svg)











