ARTICLE
Prepare Star Ratings Work Plans for the Health Equity Index
August 9, 2023

With the announcement that the Centers for Medicare & Medicaid Services (CMS) will replace the current Reward Factor with the Health Equity Index (HEI) in the 2027 Star Ratings, there are a lot of questions and concerns about how the HEI reward will operate. Securing quality bonus payments under this new direction requires an intricate understanding of what health equity means to CMS, how the measure will impact Star Ratings, and how Medicare Advantage plans can start accelerating performance today.
What is the Health Equity Index?
Through the Office of Minority Health (OMH), CMS has released a wealth of information on Health Equity Programs, including the CMS Framework for Health Equity 2022-2023 which provides the foundation and priorities for achieving health equity within government-sponsored programs.
According to the framework, CMS defines advancing health equity as striving “to identify and remedy systemic barriers to equity so that every one of the people we serve has a fair and just opportunity to attain their optimal health regardless of race, ethnicity, disability, sexual orientation, gender identity, socioeconomic status, geography, preferred language, or other factors that affect access to care and health outcomes.”
As the first step in this process, CMS will focus the HEI on social risk factors (SRF) for a subset of Star Ratings measures for members who are considered low-income subsidy (LIS) or dually eligible (DE) for Medicaid and those who qualified for Medicare due to a disability. The first HEI scores will be based on pooled data from measurement years 2024 and 2025. Now is the time to review available data, calculate projected scores, identify challenges, and set priorities.
Which Plans are Eligible for Rewards Under the HEI?
To qualify for an HEI reward, plans must meet minimum percentage thresholds for enrollment. The thresholds include:
- Full rewards for contracts with a percentage of membership with SRFs that is equal to or greater than the contract-level median SRF enrollment for all contracts, or
- Half rewards for contracts with a percentage of membership with SRF that is equal to or greater than 50% of the contract-level median SRF enrollment for all contracts but less than 100% of the contract-level median.
How Will CMS Calculate HEI Scores?
During the CMS Health Equity Conference in June 2023, CMS presented an in-depth breakdown of not only the rationale and approach behind the program, but also how CMS will calculate HEI performance and reward factors. The specific measures to be included in the HEI score will be determined each year after all data has been submitted, but Medicare Advantage plans can use the historic data provided by CMS to plan quality improvement activities and identify areas in which there may be disparity in health outcomes.
First, CMS will review contract performance on each measure for LIS, DE and disabled enrollees, and award plan points based on where they rank against other plans:
- Plans that perform in the bottom third will receive -1 point.
- Plans that perform in the middle third will receive 0 points.
- Plans that perform in the top third will receive 1 point.
These points will be multiplied by each measure’s weight to create a weighted score. Weighted scores will then be added together to create a total weighted score for a contract. CMS will then divide the total weighted score by the total measure weights to create an HEI score for a contract. Contracts that score above 0 and meet the SRF membership enrollment threshold will earn a reward.
CMS provided a simplified example of how to calculate HEI score during the presentation “An Overview of CMS-Developed Indices Measuring Health and Health Care Equity/Disparity Performance (Priority Areas 1, 2, 3, 4)” at the CMS Health Equity Conference June 6-7, 2023:
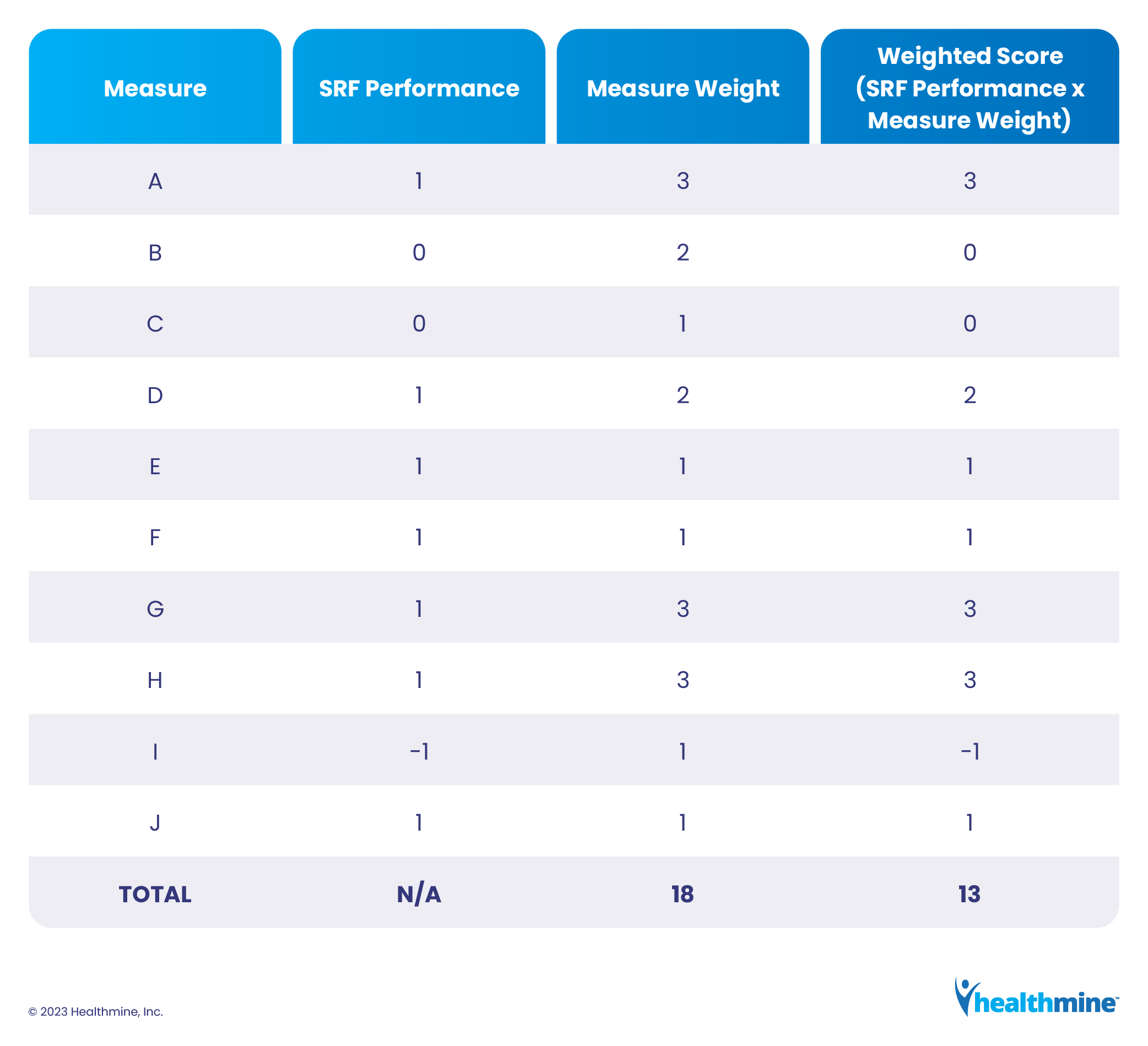
In this example, the final HEI score would be 0.722, or 13/18.
How are HEI Rewards Calculated?
CMS will use HEI scores and enrollment thresholds to determine rewards. If a plan receives an HEI score of 0 or less, they will be ineligible for rewards. Plans that achieve above 0 will receive a reward based on the following SRF enrollment thresholds:
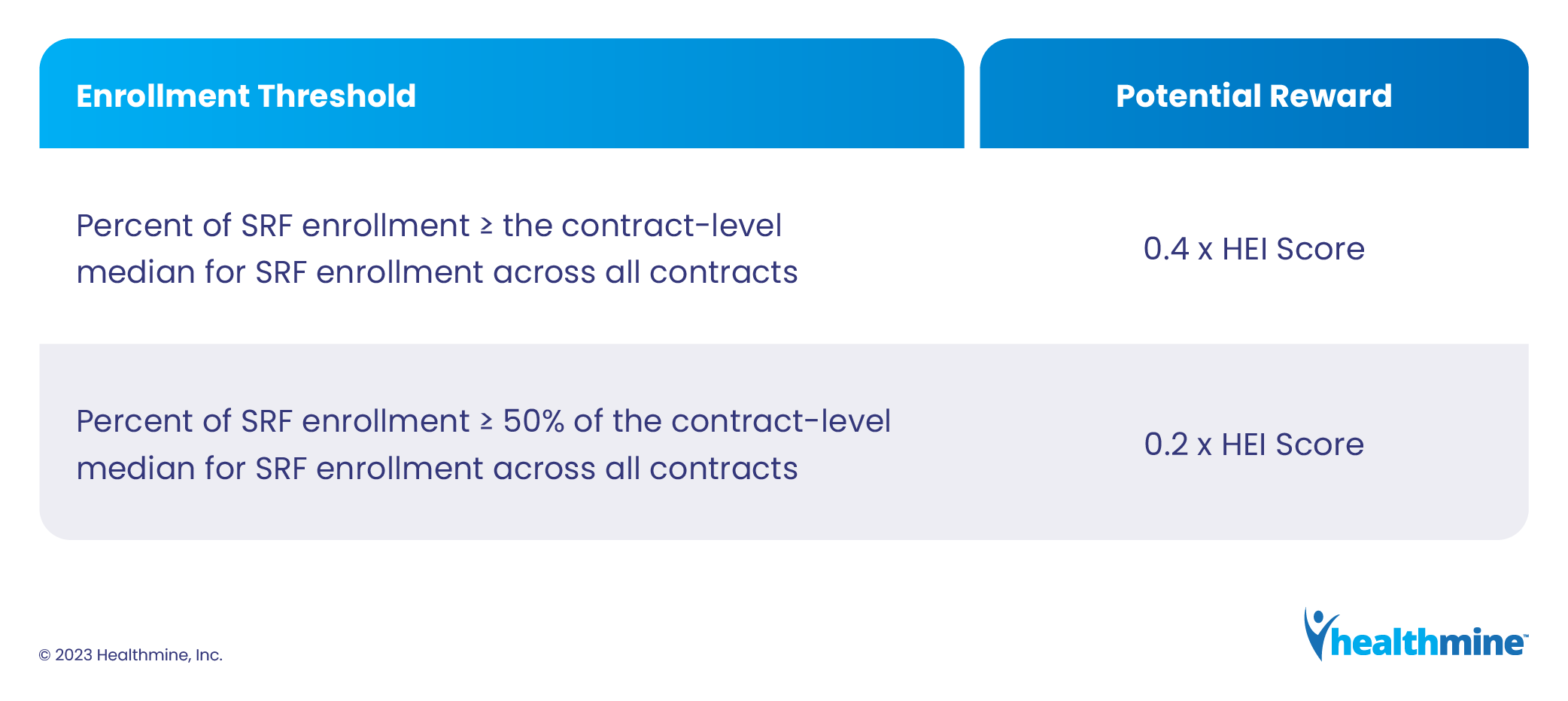
Using the earlier example from CMS, if a contract is eligible for the full reward and receives an HEI score of 0.722, it will earn a reward of 0.289, or 0.4 x 0.722.
If the contract is only eligible for half of the reward, the reward will be 0.144, or 0.2 x 0.722.
How does the HEI Reward Impact Star Ratings?
The HEI reward will replace the existing Reward Factor in providing Medicare Advantage plans additional points on their final Star Ratings. While the current Reward Factor only applies to plans with 4.0 or more Stars, the HEI will apply regardless of Star Rating if the contract meets the SRF enrollment threshold.
HEI rewards will be added to the unrounded overall Star Ratings for a contract. The Star Rating will be rounded to the nearest half Star to create the final Star Rating.
Continuing the example provided by CMS, a reward of 0.289 will be applied to the plan’s unrounded overall Star Ratings. If a plan achieves a 3.623 Star Ratings, then the reward will increase the rating to 3.912. After the final Star Rating is rounded to the nearest half Star, the contract’s final score will be 4.0 Star Ratings, the minimum threshold for quality bonus payments.
What HEI Resources are Available?
In addition to the Framework for Health Equity and details provided in the 2024 Final Rule, CMS has provided several resources to help plans prepare for HEI, including:
- The OMH Health Equity Technical Assistance Program, which contains a tool for mapping Medicare disparities along with a variety of other resources.
- A downloadable presentation covering CMS-developed indices for measuring health equity and health disparities.
- Summary data illustrating the disparities in clinical care for LIS/DE and disabled Medicare beneficiaries.
- Contract level reporting for LIS/DE and Disabled members via the Health Plan Management System (HPMS) for the following Star measures compared against national performance:
|
|
Healthmine’s Expert Advisory Services team also provided an in-depth look at the HEI and how it will impact Star Ratings in a recent webinar.
How Should I Prepare for the HEI?
First, analyze your current data. Identify your LIS/DE and disabled members and compare your performance for Star measures CMS provided in the contract-level stratified reporting via HPMS with the performance for your non-LIS/DE and disabled members.
Second, review contract-level stratified data to identify which measures for which you performed in the middle or bottom third of plans. Remember that this data is directional and does not reflect the final scores CMS will calculate. You will not know how your current performance compares to other plans until CMS releases the actual scores, but you can use this historic data to guide quality improvement strategies.
Third, determine the root causes for low performance and develop action plans to remediate the issues and achieve equitable care for your LIS/DE and disabled members.
What’s Next for Health Equity in Medicare?
LIS/DE and disabled status are just the first social risk factors CMS is using to address health equity. More are sure to come, but CMS has not shared them with plans yet. While the HEI absolutely will impact plans and the Star Ratings, the ultimate goal is to ensure all members have equal access to appropriate care. Plans that prioritize this philosophy in their Stars work plans will set themselves up for success when change inevitably comes.
According to CMS, plans should:
- Focus on providing a fair and just opportunity for every member to attain their highest level of health.
- Identify dual eligible and disabled members using monthly membership reports provided by CMS.
- Analyze current performance to ensure you are meeting the access and care needs of your most vulnerable populations.
- Identify barriers to care, including food insecurity, transportation issues, provider accessibility and language and cultural barriers.
- Remove barriers to care with community-based services, local resources, staff education and benefits.
- Look to the future and anticipate the next wave of social risk factors.
If you have questions or need help analyzing your data and developing strategies in this significant era of change, please contact me at Cherie.Shortridge@healthmine.com for more information.
